Introduction
The healthcare landscape is ever-evolving, with new policies and regulations continually shaping how care is delivered to vulnerable populations. The Consolidated Appropriations Act of 2023, specifically, Section 5121 (CAA23 -Sec. 5121) introduced new mandates that Medicaid and CHIP agencies provide essential health services to young people who are incarcerated and post-adjudication. The policy is in effect January 1, 2025. It significantly transforms the healthcare landscape, as early intervention, care coordination, and advancing peer-to-peer telehealth technologies can address cavernous gaps in mental health and related chronic conditions for vulnerable youth. The societal impact equals safer communities, reduced cost pressures on health systems, and overall long-term health as youth enter adulthood.

![]() At KemeticHlth, our commitment to communities, Medicaid populations, and healthier individual and system outcomes positions us to meet the challenge of CAA23—Sec. 5121 and model a scalable and comprehensive population health strategy that focuses on whole-person health for justice-involved youth.
At KemeticHlth, our commitment to communities, Medicaid populations, and healthier individual and system outcomes positions us to meet the challenge of CAA23—Sec. 5121 and model a scalable and comprehensive population health strategy that focuses on whole-person health for justice-involved youth.
Transformative Youth Healthcare and Innovations
The flexibility and demonstration power of the 1115 waiver and similar funding provisions will help states implement the CAA23 – Sec. 5121. Specifically, states must provide physical and behavioral health screening and diagnostic services that are medically necessary within 30 days before the scheduled release. The states must also provide targeted case management within 30 days before the planned release as well as 30 days following the release. The services include:
- assessment of individuals needs for medical, educational, social and other services;
- development of a person-centered care plan based on the results of the assessment;
- referral and connections to services to address the identified needs in the individualized care plan; and
- ongoing monitoring and follow-up activities to ensure that the care plan is effectively implemented, and needs are being met.
The Act not only mandates care during incarceration but also emphasizes the importance of continuity of care post-release. This provision recognizes the critical period following release, where the risk of health deterioration, relapse into substance use, and recidivism is high.
The 1115 Waiver presents an opportunity for developing and evaluating behavioral health technology, telehealth, and on-the-ground in-person care as a robust population health strategy that meets these new requirements and makes a profound difference in the lives of youth qualifying for Medicaid and other age/disability-related coverage.
It is estimated that 60% of youth who enter carceral settings are eligible for Medicaid and CHIP. However, historically, incarcerated youth have been marginalized in terms of healthcare access. Most enter the justice system with no formal assessment of their health care history, health-determining social needs, and trauma-informed care needs. Antiquated Medicaid Inmate Exclusion Policies prohibit and restrict the use of federal funds for any incarcerated individual, despite prior eligibility, except when they are hospitalized for 24 hours or longer. Therefore, upon entry into a carceral setting, Medicaid enrollment is terminated requiring reapplication for Medicaid coverage upon return into the community. Youth and young adults are not mentally skilled or prepared to complete these applications. Consequently, there’s disruption in continuity of care which further complicates understanding and respect for patients’ treatments while incarcerated, exacerbates existing health conditions, and increases the risk of developing new ones.
Coordinated and Peer to Peer Telehealth Care
Coordinated and peer-to-peer telehealth care under the CAA23 – Sec. 5121 facilitates location and risk reduction services for populations with complex needs. Implementation of strategies addressing determinants of health needs and re-entry-related challenges faced by incarcerated youth include:
- Integrated Care Management: At the heart of Medicaid care coordination is the ability to manage the care of individuals with multiple, complex health needs. For incarcerated youth, this means developing care plans that are not only comprehensive but also personalized. These care plans should address physical health, mental health, substance use disorders, and social determinants of health. By coordinating care across different providers and settings, innovative coordination using the 1115 Waiver can ensure that these young people receive consistent and high-quality care, both during incarceration and after release.
- Continuity of Care: One of the biggest challenges in providing healthcare to incarcerated youth is ensuring continuity of care. Innovative coordination using the 1115 Waiver can bridge the gap between the healthcare provided in the criminal justice system and the community-based care that follows the release. This involves establishing strong partnerships with correctional facilities, community health providers, and social services organizations to create a seamless transition for these young individuals as they re-enter society.
- Behavioral Health Services: Many incarcerated youth struggle with behavioral health issues, including mental health disorders and substance use disorders. State demonstration projects under the 1115 Waiver can integrate behavioral health services into the broader care plan. By providing access to therapy, counseling, and substance use treatment, these projects can address the underlying issues that often contribute to criminal behavior and help set these young people on a path to recovery.
- Data-Driven Strategies: Effective care coordination relies on data. State demonstration projects under the 1115 Waiver must leverage data to identify the specific needs of incarcerated youth, track their health outcomes, and adjust care plans accordingly. This data-driven approach ensures that care is tailored to the individual and that interventions are timely and effective.
- Community Engagement and Support: Upon release, incarcerated youth face numerous challenges, including finding stable housing, continuing their education, and securing employment. State demonstration projects under the 1115 Waiver can play a critical role in connecting these young people with community resources that support their reintegration. This holistic approach to care coordination not only addresses immediate health needs but also promotes long-term stability and well-being.
Health and Socioeconomic Needs of Justice-Involved Youth
In the United States, most children or adolescents suspected of committing a crime are placed in the jurisdiction of the juvenile justice system. The maximum age of juvenile court jurisdiction varies by state. As of 2019, 46 states have a maximum age of 17, and five states have a maximum age of 16. Some minors are processed through the criminal (adult) justice system. Justice-involved youth who are incarcerated are held in several carceral settings including short-term facilities such as detention centers, long-term secure facilities for juveniles, long-term residential facilities for juveniles, and adult jails and prisons.
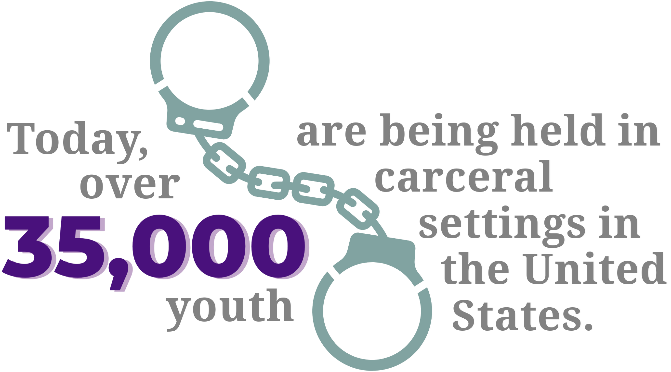
Today, over 35,000 youth are being held in carceral settings in the United States. Youth involved in the justice system often have complex and significant health, social, and economic needs. Research shows that youth who experience poor health in addition to social and economic disadvantages are more likely to become involved in the justice system and suffer from high rates of rearrests and re-incarceration. Consequently municipal, healthcare and correctional systems face escalating costs where cost savings could be reinvested in education, job training, and treatment.
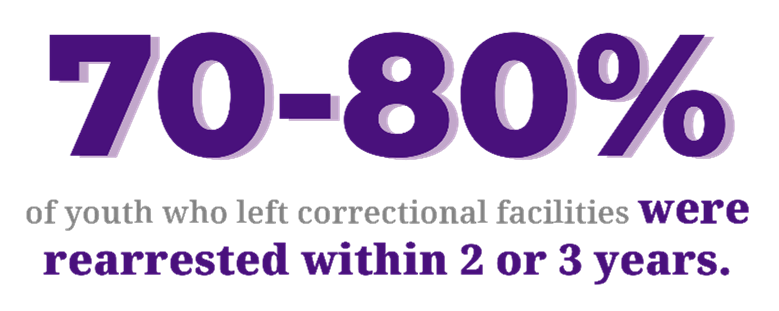
Available studies of state-by-state recidivism show that 70-80% of youth who left correctional facilities were rearrested within 2 or 3 years. A more recent study of more than 46,000 juvenile cases across 32 jurisdictions found that pretrial juvenile detention increased the likelihood of felony recidivism by 33% and misdemeanor recidivism by 11% within 1 year. Therefore, we must address not only the immediate health needs but also the social determinants of health (SDoH) to promote long-term stability and well-being among this population.
Preparing for Implementation: Key Considerations
Implementing a population health strategy that aligns with CAA23 – Sec. 5121 requires thoughtful preparation. Innovative implementation strategies must consider several factors to ensure successful execution:
- Collaboration with Stakeholders and Community Partnerships: Effective care coordination for incarcerated youth requires collaboration with a wide range of stakeholders, including correctional facilities, state Medicaid agencies, community health organizations, and social services providers. Building these partnerships is essential for creating a coordinated, comprehensive care network.
- Training and Workforce Development: The unique needs of incarcerated youth require specialized training for care coordination staff. This includes training in trauma-informed care, cultural competence, and understanding the specific challenges faced by this population. Investing in workforce development (e.g. peer to peer) ensures that staff are equipped to provide the highest level of care.
- Advocacy and Policy Engagement: State demonstration projects under the 1115 Waiver should engage in advocacy efforts to ensure that the needs of incarcerated youth are reflected in state and federal policy discussions. This includes advocating for adequate funding, resources, and support for programs that serve this population.
- Building Technological Infrastructure: Effective care coordination relies on robust technological infrastructure that supports data sharing, care plan management, and communication between providers. Investing in technology is critical to ensuring that care coordination efforts are efficient and effective.
The Path Forward
The requirements of Section 5121 of the Consolidated Appropriations Act of 2023 present a pivotal opportunity for states to lead in the implementation of a population health strategy for incarcerated youth. By leveraging expertise in care management, behavioral health integration, and community engagement, states can make a profound impact on the health and well-being of this vulnerable population. The future health outcomes of incarcerated youth depend on rising to this challenge and leading the way in transforming care, ensuring they receive the support they need to thrive both during and after their time in custody.
As we move forward, KemeticHLTH is poised to be an essential partner for care coordination innovation, collaboration, and excellence.
